您好!歡迎訪問洛陽富道生物科技有限公司官方網(wǎng)站!

Natural killer cells are the first line of defense against tumor surveillance. Currently, efforts are being made to harness the potential of NK cells as tools for immunotherapy. Rapid progress is being made in engineering NK cells for tumor immunotherapy. Chimeric antigen receptor (CAR)-engineered NK (CAR-NK) cells are gaining ground on CAR-T cells because of better safety, cytotoxic function, and high feasibility for “off-the-shelf” manufacturing. In addition, bispecific NK cell engagers (BiKEs) and trispecific NK cell engagers (TriKEs) therapy have proven beneficial in solid tumors. In this review, we will focus on recent progress in the therapeutic competence of NK cell immunotherapy, including CAR-NK and BiKE across several in vivo and in vitro models.

T75細(xì)胞培養(yǎng)瓶
自然殺傷細(xì)胞是抵御腫瘤監(jiān)視的第一道防線。目前,正在努力利用 NK 細(xì)胞作為免疫治療工具的潛力。用于腫瘤免疫治療的 NK 細(xì)胞工程正在取得快速進(jìn)展。嵌合抗原受體 (CAR) 工程化 NK (CAR-NK) 細(xì)胞由于具有更好的安全性、細(xì)胞毒性功能以及“現(xiàn)成”制造的高可行性,在 CAR-T 細(xì)胞上取得了進(jìn)展。此外,雙特異性 NK 細(xì)胞接合劑 (BiKEs) 和三特異性 NK 細(xì)胞接合劑 (TriKEs) 療法已被證明對實(shí)體瘤有益。在這篇綜述中,我們將重點(diǎn)關(guān)注 NK 細(xì)胞免疫療法的治療能力的最新進(jìn)展,包括 CAR-NK 和 BiKE 在多個(gè)體內(nèi)和體外模型中的應(yīng)用。
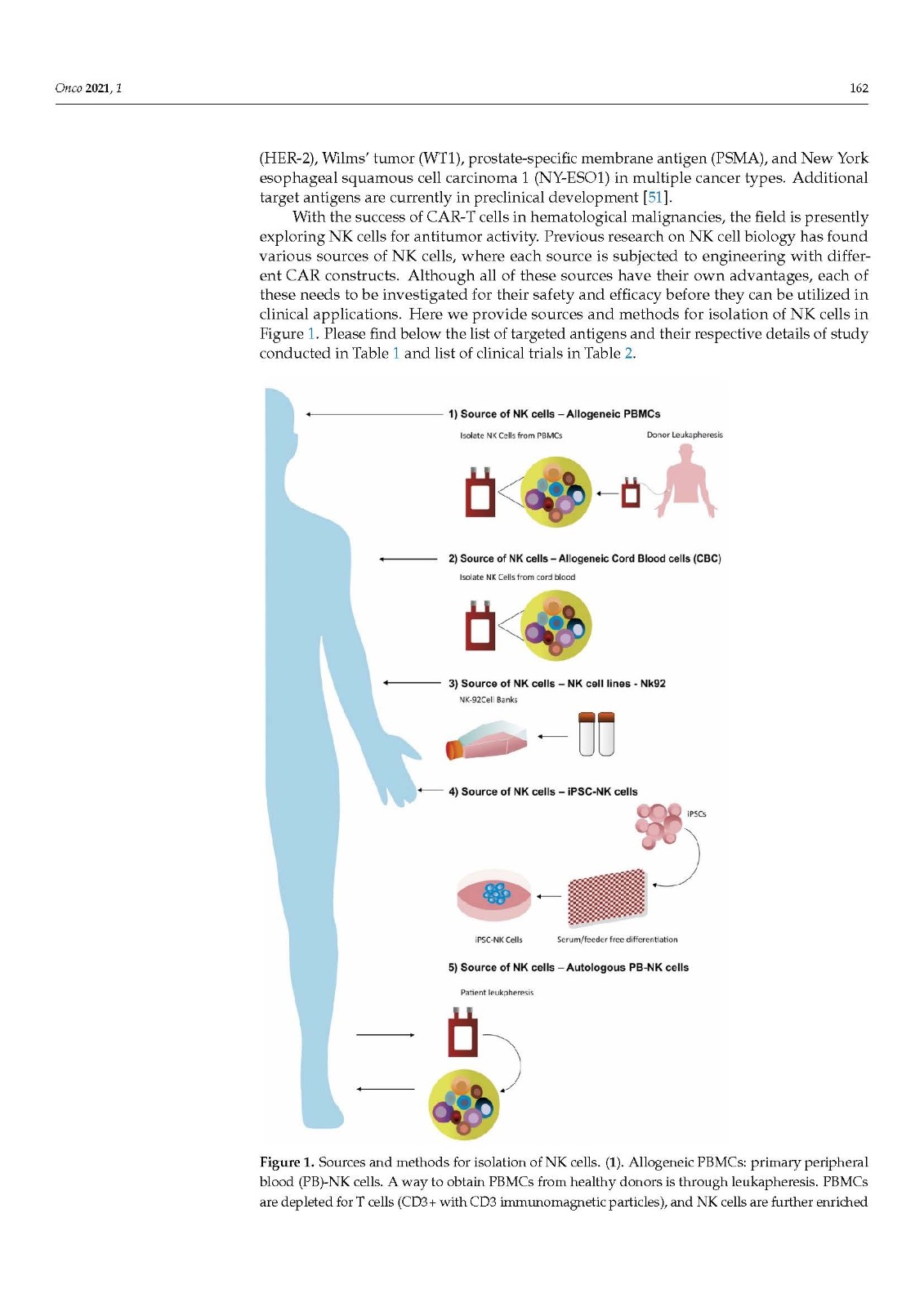
Increasing knowledge of cancer immunology has led to the design of therapies using immune cells directly or manipulating their activity, collectively termed immunotherapy. In the field of immuno-oncology, research on adaptive immune T cells has led to the development of CAR-T cells. Innate immune cells such as NK cells can also eliminate oncogenically transformed cells and regulate cells of the immune system. Considering NK cells as a live drug, numerous methods for the isolation and activation of NK cells have been shown to be clinically and therapeutically relevant. In such processes, various cytokines and antibodies present a source of stimulation of NK cells and enhance the efficacy of such treatments. The ex vivo expansion and activation of NK cells, along with genetic modification with CAR, enhance their antitumor activity. Recent preclinical studies have shown an antitumor effect through extracellular vesicles (EVs) derived from NK cells. Work with autologous NK cells has provided insights for clinical applications. In this review, we outline the recent advances of NK-cell-based immunotherapies, summarizing CAR-NK cells, BiKEs, and TriKEs as treatment options against cancer. This review also discusses the challenges of NK cell immunotherapy.
癌癥免疫學(xué)知識的增加導(dǎo)致了直接使用免疫細(xì)胞或操縱其活性的療法的設(shè)計(jì),統(tǒng)稱為免疫療法。在免疫腫瘤學(xué)領(lǐng)域,對適應(yīng)性免疫T細(xì)胞的研究帶動了CAR-T細(xì)胞的發(fā)展。天然免疫細(xì)胞如 NK 細(xì)胞也可以消除致癌轉(zhuǎn)化細(xì)胞并調(diào)節(jié)免疫系統(tǒng)細(xì)胞。將 NK 細(xì)胞視為一種活性藥物,許多分離和激活 NK 細(xì)胞的方法已被證明具有臨床和治療相關(guān)性。在這些過程中,各種細(xì)胞因子和抗體是 NK 細(xì)胞的刺激源,并增強(qiáng)了此類治療的功效。NK 細(xì)胞的體外擴(kuò)增和激活,以及 CAR 的基因改造,增強(qiáng)了它們的抗腫瘤活性。最近的臨床前研究表明,來自 NK 細(xì)胞的細(xì)胞外囊泡 (EV) 具有抗腫瘤作用。使用自體 NK 細(xì)胞為臨床應(yīng)用提供了見解。在這篇綜述中,我們概述了基于 NK 細(xì)胞的免疫療法的最新進(jìn)展,總結(jié)了 CAR-NK 細(xì)胞、BiKE 和 TriKE 作為抗癌治療選擇。本綜述還討論了 NK 細(xì)胞免疫療法的挑戰(zhàn)。

40層細(xì)胞工廠
The future of clinical trials depends on many factors—most importantly, the trial design. NK cell immunotherapies, which harness the power of NK cells, have shown promising results and are complementary to T-cell therapies. Recent advances in gene manipulation have allowed for the creation of novel CAR-NK cell products with enhanced antitumor response [25]. The clinical trials of pleiotropic CAR-NK, which have gained a lot of attention, have begun to investigate the potential of this type of cancer immunotherapy. Similar to T cells, the engineering of NK cells continues to face difficulties such as safety, clinical efficacy, homing, dose replications, and in vivo persistence after treatment. Various modes of drug delivery, including lipid nanoparticles (LPNs) and liposomes, are currently being explored for use in adoptive transfer modalities. Briefly, LPNs are composed of ionizable lipid, a cholesterol moiety, and an additional helper phospholipid and lipid-anchorage polyethylene-glycol conjugate to minimize LPN aggregation [107]. Margert et al. reported LPNs designed for ex vivo mRNA delivery to human T cells. Several ionizable lipids were produced and then formulated into LPNs. They were further used to deliver mRNA to Jurkat cells, and some formulations were capable of enhancing mRNA delivery over lipofectamine. One of the LPN formulations was further selected to deliver CAR mRNA into primary human T cells. CAR-T cells engineered with the LPN method were then compared to electroporated (EP) CAR-T cells in a coculture assay with the Nalm-6 cell line, where CAR-T cells engineered via both these methods showed pronounced antitumor activity. Overall, this report signifies the importance of an alternate delivery method of mRNA to primary human T cells through LPN which can induce functional protein expression, as well as enhance mRNA-based CAR-T cells. Further investigation is required for the ability of LPNs to deliver cargo in TME and expression patterns in solid tumors [108].
Ultimately, the goal has been to provide an “off-the-shelf” product, which is considered nontoxic to normal healthy tissues after being adoptively infused into patients. The goal further covers the product that could be delivered to all HLA haplotypes without the occurrence of GvHD. Modification of iPSCs with CRISPR technology or inclusion of novel genes to improvise persistence of CAR-NK in TME are some of the key innovations moving forward. The reprogramming of CAR-NKs to overcome tumor suppression and escape is instrumental for the clinical outcome of NK therapies. Suitable gene modification along with biomanufacturing and banking processes will require further intricate optimization. Exploration for more optimal strategies and broad-range tumor targets for solid tumors is required. Manifestations of all these efforts are primarily aimed to avoid off-target cytotoxicity.

高效搖瓶5L
臨床試驗(yàn)的未來取決于許多因素——最重要的是試驗(yàn)設(shè)計(jì)。利用 NK 細(xì)胞的力量的 NK 細(xì)胞免疫療法已顯示出有希望的結(jié)果,并且是 T 細(xì)胞療法的補(bǔ)充。基因操作的最新進(jìn)展允許創(chuàng)造具有增強(qiáng)抗腫瘤反應(yīng)的新型 CAR-NK 細(xì)胞產(chǎn)品 [ 25]]。備受關(guān)注的多效性CAR-NK的臨床試驗(yàn),已經(jīng)開始探索這種癌癥免疫療法的潛力。與 T 細(xì)胞類似,NK 細(xì)胞的工程化繼續(xù)面臨安全性、臨床療效、歸巢、劑量復(fù)制和治療后體內(nèi)持久性等困難。目前正在探索各種藥物遞送模式,包括脂質(zhì)納米顆粒 (LPN) 和脂質(zhì)體,以用于過繼轉(zhuǎn)移模式。簡而言之,LPN 由可電離的脂質(zhì)、膽固醇部分和額外的輔助磷脂和脂質(zhì)錨定聚乙二醇共軛物組成,以最大限度地減少 LPN 聚集 [ 107]]。瑪格特等人。報(bào)道了設(shè)計(jì)用于將 mRNA 離體傳遞到人類 T 細(xì)胞的 LPN。產(chǎn)生了幾種可電離的脂質(zhì),然后將其配制成 LPN。它們被進(jìn)一步用于將 mRNA 遞送至 Jurkat 細(xì)胞,并且一些制劑能夠增強(qiáng) mRNA 遞送而不是 lipofectamine。進(jìn)一步選擇了一種 LPN 制劑將 CAR mRNA 遞送到原代人類 T 細(xì)胞中。然后在與 Nalm-6 細(xì)胞系的共培養(yǎng)試驗(yàn)中,將用 LPN 方法改造的 CAR-T 細(xì)胞與電穿孔 (EP) CAR-T 細(xì)胞進(jìn)行比較,其中通過這兩種方法改造的 CAR-T 細(xì)胞顯示出明顯的抗腫瘤活性。總的來說,這份報(bào)告表明了一種通過 LPN 將 mRNA 傳遞給原代人類 T 細(xì)胞的替代方法的重要性,該方法可以誘導(dǎo)功能性蛋白質(zhì)表達(dá),并增強(qiáng)基于 mRNA 的 CAR-T 細(xì)胞。108 ]。
最終,目標(biāo)是提供一種“現(xiàn)成的”產(chǎn)品,這種產(chǎn)品在被過繼注入患者體內(nèi)后被認(rèn)為對正常健康組織無毒。該目標(biāo)進(jìn)一步涵蓋了可以在不發(fā)生 GvHD 的情況下交付給所有 HLA 單倍型的產(chǎn)品。使用 CRISPR 技術(shù)修改 iPSC 或包含新基因以提高 CAR-NK 在 TME 中的持久性是一些關(guān)鍵創(chuàng)新。CAR-NKs 的重編程以克服腫瘤抑制和逃逸對 NK 療法的臨床結(jié)果有幫助。合適的基因修飾以及生物制造和銀行流程將需要進(jìn)一步復(fù)雜的優(yōu)化。需要探索針對實(shí)體瘤的更優(yōu)化策略和更廣泛的腫瘤靶點(diǎn)。
關(guān)鍵詞:natural killer (NK) cells,cancer,immunotherapy,chimeric antigen receptor (CAR)-NK,iPSCs,bispecific T-cell engagers (BiKEs),trispecific NK cell engagers (TriKEs),自然殺傷(NK)細(xì)胞,癌癥,免疫療法,嵌合抗原受體 (CAR)-NK,iPSC,雙特異性 T 細(xì)胞接合器 (BiKE),三特異性 NK 細(xì)胞接合器 (TriKE)






來源:MDPI https://www.mdpi.com/2673-7523/1/2/13/htm